Pediatric Physical Therapy
Kids are fun to work with at any age. We love having fun while challenging them to get their best functional and developmental outcome.
There are many situations in which children need OT/PT services. Below are some discussions.
Developmental Delay
Delopmental delay is when a child is not able to perform functions that other children their age are typically able to perform. Developmental milestones are social, cognitive and gross and fine motor skills that a child acquires at various age ranges. For example, walking normally begins between 8 and 18 months. Below is a map of sample social, cognitive and motor developmental milestones by the Center for Disease Control (CDC).
Other motor milestones, per the US National Library of Medicine, are as follows:
Age 0 to 1 year:
Roll lefts and roll right
Sits without assist
Able to pull to standing position
Walks while holding onto furniture
Age 1 to 3 years:
Walks independently
Able to run, pivot and walk backwards
Pedals tricycle
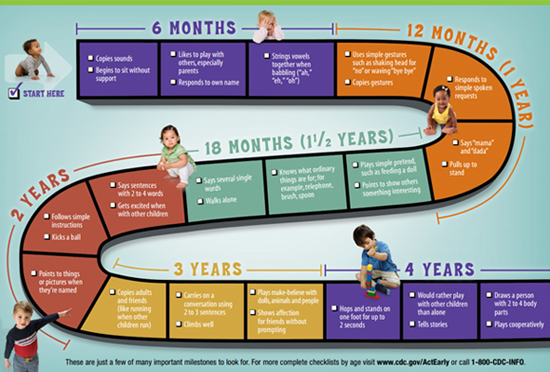
Age 3 to 6 years:
Able to Skip
Catches a bounced ball
Hops on one foot
Age 6 to 12 years:
Gains skills for team sports like soccer and volleyball
(US National Library of Medicine)
Several diagnoses are associated with developmental delay including:
- Cerebral Palsy
- Spina Bifida
- Down Syndrome
- Congenital Heart Defects
- Autism
- Trauma
- Muscular Dystrophy
- Arthrogryposis
- Torticollis
Interventions for developmental delay include:
- Facilitation for each transitions
- Increasing opportunities for using arms/ hands/ legs for play
- Positioning for facilitationof motor development
- Walking practice/ Gait training with/without orthotics
- Exercises to improve strength, range of motion, tone and endurance
- Activities to improve balance and coordination
- Sensory integration
- Patient/caregiver education
Cerebral Palsy
Cerebral Palsy is a non-progressive lesion in the infant brain that disturbs the development of posture and motor control. This group of disorders is the leading cause of disability in children. One in 323 children have cerebral palsy (NIH 2017). Cerebral palsy can be classified by extremity involvement (diplegic, hemiplegic or quadriplegic) or by motor control (spastic, hypotonic, ataxic or athetoid) or by severity (mild, moderate, severe).
Complications of Cerebral Palsy include:
- Spasticity
- Dislocations
- Paralysis
- Inability to control movements
- Inability to crawl or walk or run
- Weakness
- Cognitive
- Scoliosis
In a systematic review of 64 different interventions, the following were proven to be amongthe best treatments for children with cerebral palsy (Novak 2013).
- Bimanual coordination training
- Constraint-induced movement therapy for hemiplegia
- Context-focused therapy
- Goal-directed/functional training
- Home exercise programs for improving motor activities or self-care function
Torticollis
Torticollis is tilting of the head to one side due to sustained contraction, spasm, of the sternocleidomastoid muscle. It is important for daily caregivers to recognize signs of torticollis. The earlier the detection, the better the outcomes and the shorter duration of treatment. Torticollis is best treated within the first 2 months of life. Signs of torticollis include (Kaplan 2013):
- Stiff or large neck muscles
- Limited movement of the head
- Persistently turned head
- Asymmetry
- The top of the head may be flat
Effective treatment for torticollis includes:
- Passive, pain-free, stretching of musculature by a physical therapist
- Facilitation of symmetrical movements through righting reactions
- Arms/ shoulders/ trunk symmetrical movement pattern practice
- Environmental modification to encourage neck motion to the affected side
- Caregiver education, including "tummy time"
Torticollis left untreated may cause tingling and numbnessdue to nerve root compression.
Spina Bifida (Myelomeningocele)
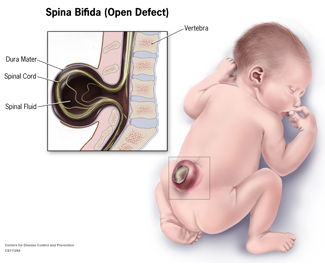
Spina bifida (myelomeningocele) is a neural tube defect in which the fetal spinal cord fails to close during the first month of pregnancy, thereby causing nerve and spinal cord damage at the level of the lesion. Spina bifida may affect continence, sensation, muscle tone and motor control.
Most children with myelomeningocele will learn to walk by 6 years old. According to research, participation in a physical therapy program committed to walking is a strong predictor of ambulation in children with spina bifida (Bartonek 2010).Prognosis for ambulation also depends on the neurological status of the patient, including spasticity, tethering of the spinal cord and extent of nerve damage.
Occupational and Physical Therapy includes therapeutic play and ADL's, activities of daily living such as transfers, walking, getting dressed, donning braces, and arts/ crafts, functional tasks for hands and trunk control.
Gait training and standing weight bearing is a major factor for long term independence.
Fractures
Fractures are most common in children and the elderly. One in 3 children will have a fracture by the age of 17. The most common site of fracture in children is the distal forearm, and the usual mechanism of injury is a fall during sports or play (Hedstrom 2010). Inability to bear weight is a sign of fracture. Other signs include inability to hold items or use the arm. Seek immediate medical attention if fracture is suspected.
Treatment for fractures include:
- Casting
- Stretching
- Strengthening
- Progressive therapeutic activities
- Modifying tasks, functional play while healing
There are many more diagnosis that we work with such as Muscular Dystrophies, strokes, metabolic diseases with functional impairments.
Call 813-631-9700 to schedule an evaluation with our OT/PT. Have a nice day!
Bibliography
Bartonek, Asa. "Motor Development Toward Ambulation in Preschool Children with Myelomeningocele." LWW, journals.lww.com/pedpt/Fulltext/2010/02210/Motor_Development_Toward_Ambulation_in_Preschool.8.aspx. Accessed 16 Aug. 2017.
"Developmental milestones record." MedlinePlus Medical Encyclopedia, medlineplus.gov/ency/article/002002.htm. Accessed 16 Aug. 2017.
Hedström, Erik M, et al. "Epidemiology of fractures in children and adolescents: Increased incidence over the past decade: a population-Based study from northern Sweden." ActaOrthopaedica, Informa Healthcare, Feb. 2010, www.ncbi.nlm.nih.gov/pmc/articles/PMC2856220/. Accessed 17 Aug. 2017.
Kaplan, Sandra, et al. "Physical Therapy Management of Congenital Muscular... : Pediatric Physical Therapy." LWW, journals.lww.com/pedpt/Fulltext/2013/25040/Physical_Therapy_Management_of_Congenital_Muscular.2.aspx. Accessed 18 Aug. 2017
Novak, Iona, et al. "A systematic review of interventions for children with cerebral palsy: state of the evidence." Developmental Medicine & Child Neurology, 21 Aug. 2013, onlinelibrary.wiley.com/doi/10.1111/dmcn.12246/full. Accessed 16 Aug. 2017.
Verschuren, Olaf "Exercise Training Program in Children and Adolescents With Cerebral Palsy." Archives of Pediatrics & Adolescent Medicine, American Medical Association, 1 Nov. 2007, jamanetwork.com/journals/jamapediatrics/fullarticle/569943 Accessed 16 Aug. 2017.
Milestone chart: https://www.cdc.gov/ncbddd/actearly/pdf/parents_pdfs/mo-wic-broch_2_english_508.pdf


